Claire Kilpatrick (left),
Consultant, World Health Organization (WHO) Service Delivery and Safety Department, Infection Prevention and Control Global Unit, Geneva, Switzerland, and Honorary Research Fellow, Imperial College London (Faculty of Medicine) and Didier Pittet (right), Director, Infection Control and The WHO Collaborating Centre on Patient Safety, University of Geneva Hospitals and Faculty of Medicine, Geneva, Switzerland, and Lead Adviser, WHO Patient Safety Clean Care is Safe Care and The African Partnerships for Patient Safety Programmes
As resistance to antibiotics becomes more common and a significant global burden, the role of hand hygiene in infection prevention and control (IPC) becomes ever more essential in preventing the spread of resistance and subsequent overuse of antibiotics. The best way to protect patients from microorganism cross-transmission is to apply a multimodal improvement strategy within healthcare systems to enhance hand hygiene action at the point of patient care (1). Compliance with recommended hand hygiene practices remains unacceptably low worldwide. Even in high-income countries with resources available for supplies, training and promotion programmes, average compliance reported in a 2010 review of available studies was approximately 40% (2). The World Health Organization (WHO) launched and executed the First Global Patient Safety Challenge, “Clean Care is Safer Care”, between 2005–2015 with the aim of targeting healthcare-associated infection (HAI) reduction, primarily through hand hygiene action.
Each year, hundreds of millions of patients around the world are affected by HAI. Understanding and assessing the global burden of HAI was one of the key areas of work of the WHO “Clean care is safer care” programme. Systematic reviews of the literature were conducted which led to the WHO Report on the burden of endemic healthcare-associated infection worldwide (3), as well as a publication on the magnitude of the problem in both developed and developing countries (4). Additionally, surveys have been conducted on understanding the burden of multidrug-resistant organisms among inpatients and surgical antibiotic prophylaxis prescribing in healthcare (5). These add to the wealth of literature available on the global burden of antimicrobial resistance (AMR).
An article concerning United States healthcare facilities participating in the WHO global campaign “SAVE LIVES: Clean Your Hands” highlighted that almost 42% still lack a team formally dedicated to hand hygiene activities (6). A WHO report in 2012 also confirmed that progress with improvement is variable around the globe (7).
Common ongoing challenges
Hand hygiene is a simple and cost-effective intervention, but in the years since the chapter on behavioural considerations in the WHO Guidelines on Hand Hygiene in Healthcare (8) was published, it has become increasingly clear that it is a behaviourally-driven science. Goal-setting, award incentives and accountability have recently been highlighted as specifically important in achieving a safety climate (9), while addressing different combinations of determinants is deemed definitively important (10). Improved behavioural strategies need to be further investigated to understand the corrective leverage necessary to stimulate change at local level. Patients have a voice too and the role of patient participation can be a powerful approach to achieve improvements in healthcare by building and strengthening a strong patient safety climate (11,12,13), but there are many cultural aspects to be taken into consideration. Finally, useful economic evidence for public health practitioners, service commissioners, and government officials on the effectiveness of a hand hygiene improvement strategy will be increasingly important, to convince them to allocate resources in a competing world of health system strengthening.
Going global to improve infection prevention and control (IPC) and prevent healthcare-associated infection (HAI)
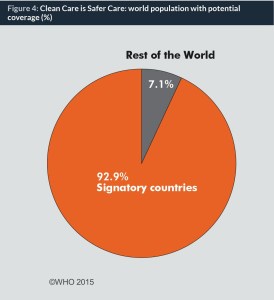
The “Clean care is safer care” global programme was based around a change model with three objectives (see Figure 1). It fostered partnerships and coordinated activities as set out in its programme plan (14). By May 2015, 139 of the 194 United Nations’ Member States had pledged their support to implement actions to reduce HAI, corresponding to 95% coverage of the world population (Figure 2). The finalized WHO Guidelines on Hand Hygiene in Healthcare was launched (8) in 2009 alongside a tried and tested multimodal improvement toolkit (1). The improvement strategy, and therefore the toolkit, comprises five critical components: (i) system change; (ii) healthcare workers’ training and education; (iii) evaluation and feedback; (iv) reminders in the workplace; and (v) promotion of an institutional safety climate. Additionally, WHO has over this time coordinated more than 50 national campaigns and, importantly, launched the global annual healthcare worker call to action; the “SAVE LIVES: Clean Your Hands campaign” (15), to maintain a profile on hand hygiene action at the point of care. By November 2015, almost 19,000 healthcare facilities had registered their commitment to action.
Box 1: 140 Countries committed to addressing HCAI (as of January 2015)
Americas region: Argentina, Bolivia, Brazil, Canada, Chile, Colombia, Costa Rica, Cuba, Dominican Republic, El Salvador, Ecuador, Guatemala, Honduras, México, Nicaragua, Panama, Paraguay, Peru, United States of America, Uruguay and 14 Caribbean States (34)
Eastern Mediterranean region: Afghanistan, Bahrain, Egypt, Islamic Republic of Iran, Jordan, Kingdom of Saudi Arabia, Kuwait, Lebanon, Sultanate of Oman, Tunisia, Pakistan, Sudan, Qatar, United Arab Emirates, Yemen (15)
European region: Austria, Belarus, Belgium, Bulgaria, Croatia, Cyprus, Denmark, Finland, France, Germany, Georgia, Greece, Hungary, Iceland, Ireland, Italy, Kazakhstan, Kyrgyzstan, Luxembourg, Malta, Republic of Moldova, the Netherlands, Norway, Poland, Portugal, Russian Federation, Serbia, Slovenia, Spain, Sweden, Switzerland, Tajikistan, United Kingdom of Great Britain and Northern Ireland (33)
South East Asian region: Bhutan, Bangladesh, India, Indonesia, Myanmar Thailand (6) West Pacific region: Australia, China, Cambodia, Japan, Laos, South Korea, Malaysia, Mongolia, New Zealand, the Philippines, Singapore, Viet Nam, HK, Tonga (14)
© World Health Organization
Ten years of “Clean care is safer care”
As well as country pledges, facility registrations and national campaigns, described here are other achievements of the “Clean care is safer care” programme:
- “Clean care is safer care” work has put a focus on patient engagement as a way of tackling hand hygiene improvement and WHO has issued patient engagement guidance and tools in conjunction with experts (8,16).
- Many articles have been published by a large group of authors, including those initiated under the leadership of “Clean care is safer care”, which can persuade health workers of the continued need for hand hygiene action. In 2010, trends in publication dynamics were presented, comparing hand hygiene with other health-related topics in publication (17).
- Seven years of “SAVE LIVES: Clean Your Hands” have seen a range of foci in order to maintain engagement, including new posters, surveys and relationship building. WHO has also emphasized that hand hygiene is not a standalone action. In 2014, posters and educational messages were created to emphasize the role of hand hygiene in antimicrobial resistance (18).
- In 2015, a massive surge of interest in and commitment to hand hygiene was again seen through the campaign in the form of #safeHANDS, when thousands of people sent a strong message across the world. The global reach was approximately 50 million, based on social media analytics.
- Between 5 May and 5 September 2015, hospitals and healthcare institutions worldwide were invited to participate in “Hand Sanitizing Relays” by the WHO Collaborating Centre on Patient Safety at the University of Geneva Hospitals. The Relays consisted of chains of healthcare care workers rubbing their hands according to the WHO ”How to Handrub” technique (19) and passing the alcohol-based handrub on from hand to hand. This activity engaged more than 30,000 staff worldwide and ensured a large mobilization from participating healthcare settings (20). This initiative was modelled on the action proposed by the Hong Kong Baptist Hospital who established a new Guinness World Record on 5 May 2014 with 266 staff involved in a Hand Sanitizing Relay. When assessed before and after the relay, overall compliance with hand hygiene was shown to improve institution-wide, as outlined by Seto et al (21).
- WHO’s alcohol-based handrub formulation was added to the WHO Essential Medicine List in 2015 which aimed to have an impact in low- and middle-income countries in particular (22).
- An initiative called ”Private Organizations for Patient Safety” (POPS) was launched to support capacity-building and global reach in healthcare hand hygiene improvement. With the aim of engaging with private industry companies with a focus on corporate social responsibility, POPS has already delivered on a number of projects (23).
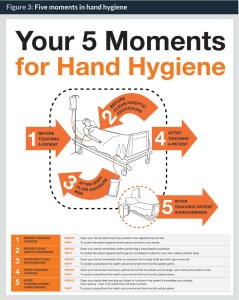
WHO’s “My 5 Moments for Hand Hygiene”: The foundation of action at the point of patient care to ensure successful IPC
The “My 5 Moments for Hand Hygiene” approach (24), developed at the University of Geneva Hospitals, Switzerland, defines the key moments when healthcare workers should perform hand hygiene and is intended to meet the needs for training, observation, and performance reporting across all healthcare settings worldwide (Figure 3). This is an evidence-based, field-tested, user-centred approach and it recommends healthcare workers to clean their hands before touching a patient; before clean/aseptic procedures; after body fluid exposure/risk; after touching a patient; and after touching patient surroundings.
An additional concept critical to the understanding of hand hygiene requirements is the term “point of care”. The “point of care” is exactly where the care action takes place and is defined as “the place where three elements come together: the patient, the healthcare worker, and care or treatment involving contact with the patient”. Although the basic principles of IPC and hand hygiene are the same in all healthcare settings worldwide, outpatient care also presents specific challenges related to the application of the WHO “My 5 Moments for Hand Hygiene” approach. Several questions have emerged about the transmission and infection risks and the application of hand hygiene concepts in these settings, which led to an additional WHO publication focused on the application of the “My 5 Moments for Hand Hygiene” in outpatient care, home-based care and long-term care facilities (25).
Considering that the point of care is where organisms, resistant to antibiotics or not, are most likely to enter the systems of vulnerable patients, enhanced understanding and application of the “My 5 Moments for Hand Hygiene” is still critical as part of IPC programmes.
Conclusions
Although much has been achieved through the ten years of “Clean care is safer care”, going forward WHO remains committed to IPC, including maintaining a profile on hand hygiene improvement given the past ten years experience of understanding behaviour change and implementation science. This is critical given the antimicrobial reisitence burden, ongoing HAI incidence and recent outbreak situations. With a mission of “driving IPC to the top of the agenda in all countries by providing innovative, effective technical guidelines and strong coordination, with the goal of reducing infections and antimicrobial resistance in healthcare and revolutionizing the way IPC is applied” the new WHO Global Unit on IPC will focus on a range of technical areas of work. Until healthcare leaders truly accept that hand hygiene and other elements of IPC are fundamental to quality care and should be used as key quality indicators, avoidable harm will continue. Other emerging disciplines are gaining traction in the field of infection prevention, for example, human factors. Such work could play a role in behaviour change if leaders and the infection prevention community engage with those, for example, in the social sciences (26).
Hand hygiene is one of the top ten patient safety strategies ready for adoption now (27). Together people around the world can continue to reduce avoidable harm by averting the spread of diseases caused by viruses and bacteria, including those resistant to antibiotics, to patients and health workers.
Biographies
Professor Didier Pittet, MD, MS, CBE, is the Director of Infection Control & WHO Collaborating Centre on Patient Safety, Geneva, Switzerland, and Lead Adviser of the WHO Patient Safety Clean Care is Safe Care and the African Partnerships for Patient Safety programmes. He holds Honorary Professorships in London, Hong Kong, and Shanghai and is the recipient of several international honours including a CBE awarded by Her Majesty Queen Elizabeth II (2007). He is co-author of more than 500 peer-reviewed papers and 50 textbook chapters and an Editorial Consultant for the Lancet. The book “Clean Hands Save Lives” and the movie “Clean Hands” describe Didier Pittet’s medical odyssey to promote patient safety worldwide.
To download article click here
References
1. Allegranzi B, Gayet-Ageron A, Damani N et al Global implementation of WHO’s multimodal strategy for improvement of hand hygiene: a quasi-experimental study The Lancet Infectious Diseases 2013 13:10, p843–851
2. Erasmus V, Daha T, Brug H, et al Systematic review of studies on compliance with hand hygiene guidelines in hospital care. Infection Control and Hospital Epidemiology 2010; 31:283-294.
3. World Health Organization. WHO Report on the burden of endemic health care-associated infection in worldwide. 2011 Available from http://apps.who.int/iris/bitstream/10665/80135/1/9789241501507_eng.pdf?ua=1&ua=1 (accessed 31 December 2015)
4. Allegranzi B, Bagheri-Nejad S, Combescure C, et al Burden of endemic health-care-associated infection in developing countries: systematic review and meta-analysis The Lancet 2011 377:9761, p228–241
5. World Health Organization. WHO Laboratory-based global survey on MDROs – interim analysis and Global survey on surgical antibiotic prophylaxis in health care – interim analysis. 2014 Available from http://www.who.int/gpsc/5may/global-surveys_interim-results.pdf?ua=1 (accessed 31 December 2015)
6. Allegranzi B, Conway L, Larson E, Pittet D. Status of the implementation of the World Health Organization multimodal hand hygiene strategy in United States of America healthcare facilities. American Journal of Infection Control 2014 2014; 42(3):224-30.
7. World Health Organziation. WHO Hand Hygiene Self-Assessment Framework Global Survey Summary Report. 2012 Available from http://www.who.int/gpsc/5may/summary_report_HHSAF_global_survey_May12.pdf?ua=1 (accesssed 31 December 2015)
8. World Health Organization. Guidelines on Hand Hygiene in Health Care. Geneva: World Health Organization. 2009 Available from: http://whqlibdoc.who.int/publications/2009/9789241597906_eng.pdf (Accessed 31 December 2015)
9. Luangasanatip N, Hongsuwan M, Limmathurotsakul D, et al Comparative efficacy of interventions to promote hand hygiene in hospital: systematic review and network meta-analysis British Medical Journal. 2015;351:h3728. doi: 10.1136/bmj.h3728
10. Huis A, van Achterberg T, de Bruin M, et al A systematic review of hand hygiene improvement strategies: a behavioural approach Implementation Science 2012; 14;7:92
11. Longtin Y, Sax H, Leape L, et al Patient Participation: Current Knowledge and Applicability to Patient Safety Mayo Clinical Proceedings. 2010 Jan; 85(1): 53–62. doi: 10.4065/mcp.2009.0248
12. Landers T, Abusalem S, Coty M-B, Bingham J. Patient-centered hand hygiene: The next step in infection prevention American Journal of Infection Control 40 (2012) S11-S17
13. World Health Organization. Patients have a voice too! Available from http://www.who.int/gpsc/5may/5may2013_patient-participation/en/ (accessed 31 Dec 2015)
14. Pittet D, Donaldson L. “Clean care is safer care”: a worldwide priority. Lancet 2005;366:1246-1247
15. Kilpatrick C Save lives: clean your hands. A global call for action at the point of care. American Journal of Infection Control. 2009 May;37(4):261-2. doi: 10.1016/j.ajic.2009.02.001.
16. World Health Organization. Tools for Institutional Safety Climate Available from http://www.who.int/gpsc/5may/tools/safety_climate/en/ (accessed 31 December 2015)
17. Graafmans W, Kilpatrick C, Mathai E et al Trends in Scientific Publications as an Indicator for Hand Hygiene Awareness 50th Interscience Conference on Antimicrobial Agents and Chemotherapy; Boston, USA, 12-15 September 2010. (Poster)
18. World Health Organization. WHO 5 Moments Posters for Hand Hygiene in preventing the spread of MDROs Available from http://www.who.int/gpsc/5may/5moments-posters/en/ (accessed 31 December 2015)
19. World Health Organization. How to Hand Rub Available from http://www.who.int/gpsc/5may/How_To_HandRub_Poster.pdf?ua=1 (accessed 31 December 2015)
20. Tartari E, Pires D, Borzykowski T et al The Global Hand Sanitizing Relay: promoting hand hygiene through innovation. Submitted to the 26th European Congress of Clinical Microbiology and Infectious Diseases, Amsterdam April 2016
21. Seto WH, Cowling B, Cheung C, et al Impact of the first hand sanitizing relay world record on compliance with hand hygiene in a hospital American Journal of Infection Control 2015 March 43:3, Pgs 295–297
22. World Health Organization. 19th WHO Model List of Essential Medicines Available from http://www.who.int/medicines/publications/essentialmedicines/EML2015_8-May-15.pdf?ua=1 (accessed 31 December 2015)
23. World Health Organization. Private Organizations for Patient Safety Available from http://www.who.int/gpsc/pops/en/ (accessed 31 December 2015)
24. Sax H, Allegranzi B, Uckay I, et al ‘My five moments for hand hygiene’: a user-centred design approach to understand, train, monitor and report hand hygiene. Journal of Hospital Infection 2007;67:9-21
25. World Health Organization. Hand hygiene in outpatient care, home-based care and long- term care facilities 2012. Available from http://apps.who.int/iris/bitstream/10665/78060/1/9789241503372_eng.pdf?ua=1 (accessed 31 December 2015)
26. Storr J, Wigglesworth N, Kilpatrick C. Integraing human factors with infection prevention and control The Health Foundation: London (2013). Available from (accessed 31 December 2015)
27. Shekelle P, Pronovost P, Wachter R, et al The Top Patient Safety Strategies That Can Be Encouraged for Adoption Now Annals of Internal Medicine 2013; 158: 5 Part 2